
Touchless Prior Auth
We start by making existing prior authorizations fully touchless. Rhyme processes over 4M prior auths for 83 of the largest providers each year.
Touchless Prior Auth
We start by making existing prior authorizations fully touchless. Rhyme processes over 4M prior auths for 83 of the largest providers each year.
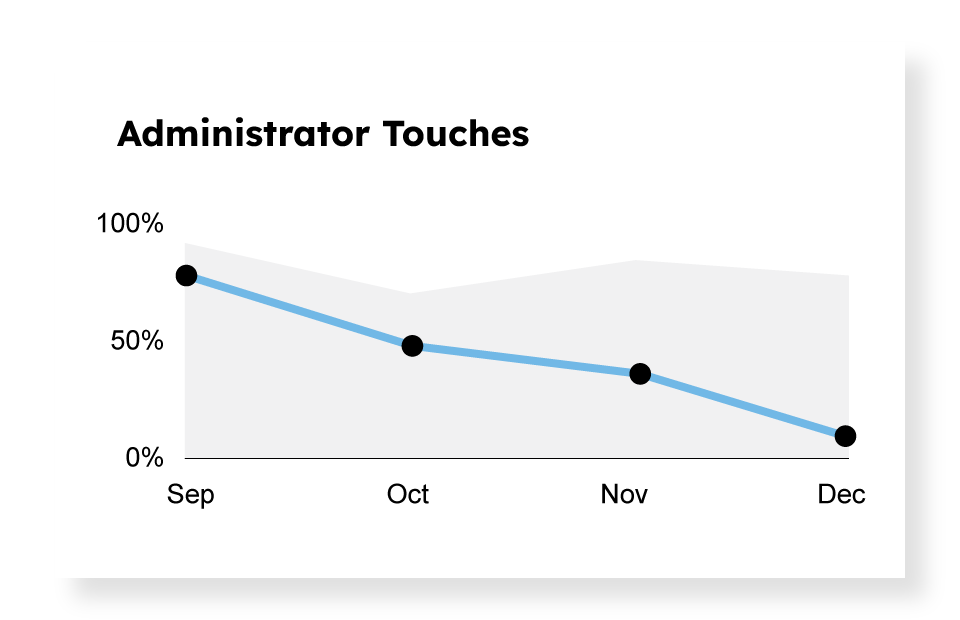
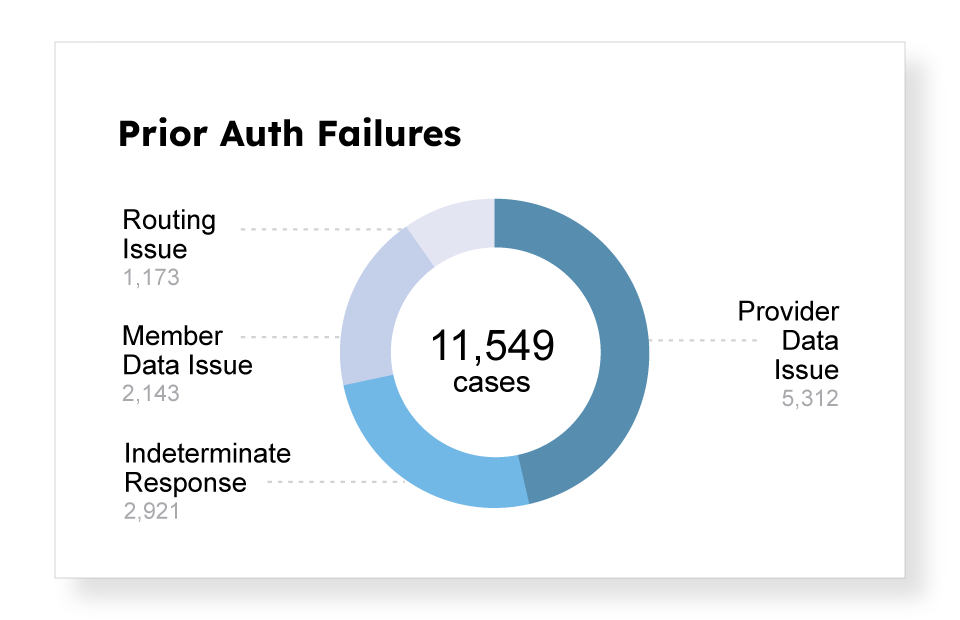
Observation is Key
Rhyme meticulously tracks the end-to-end prior auth process and automatically removes unnecessary manual effort, friction, and waste.
Gold Carding
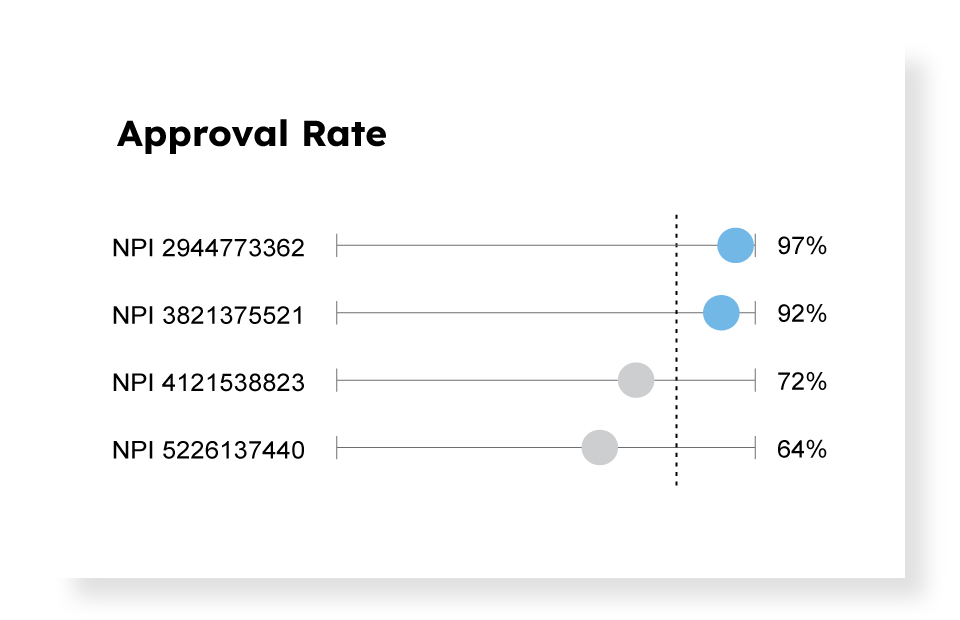
With Rhyme’s proprietary data and tools, payers and providers work together to eliminate prior auths entirely at point of care.
Gold Carding
With Rhyme’s proprietary data and tools, payers and providers work together to eliminate prior auths entirely at point of care.
Shared Dashboard
Rhyme’s visualization suite clearly observes manual effort, friction and waste. Our trusted third party tools allow payers and providers to collaborate and have a shared view of success.

Everyone Benefits
Patient
Faster time to care
with fewer denials
with fewer denials
Provider
Millions of dollars saved and more freedom to make care decisions
Payer
Improved provider
and patient satisfaction
and patient satisfaction
4M+
auths in the EHR yearly
300+
of the largest payers
83
of the largest health systems
100%
of procedure types
" Rhyme’s technology is structured to head off the challenges before they begin, and it keeps our process a lot smoother. It’s a big relief and time-saver for our staff. "
Norton Hospital
Charlotte Ekart, System Director Patient Access